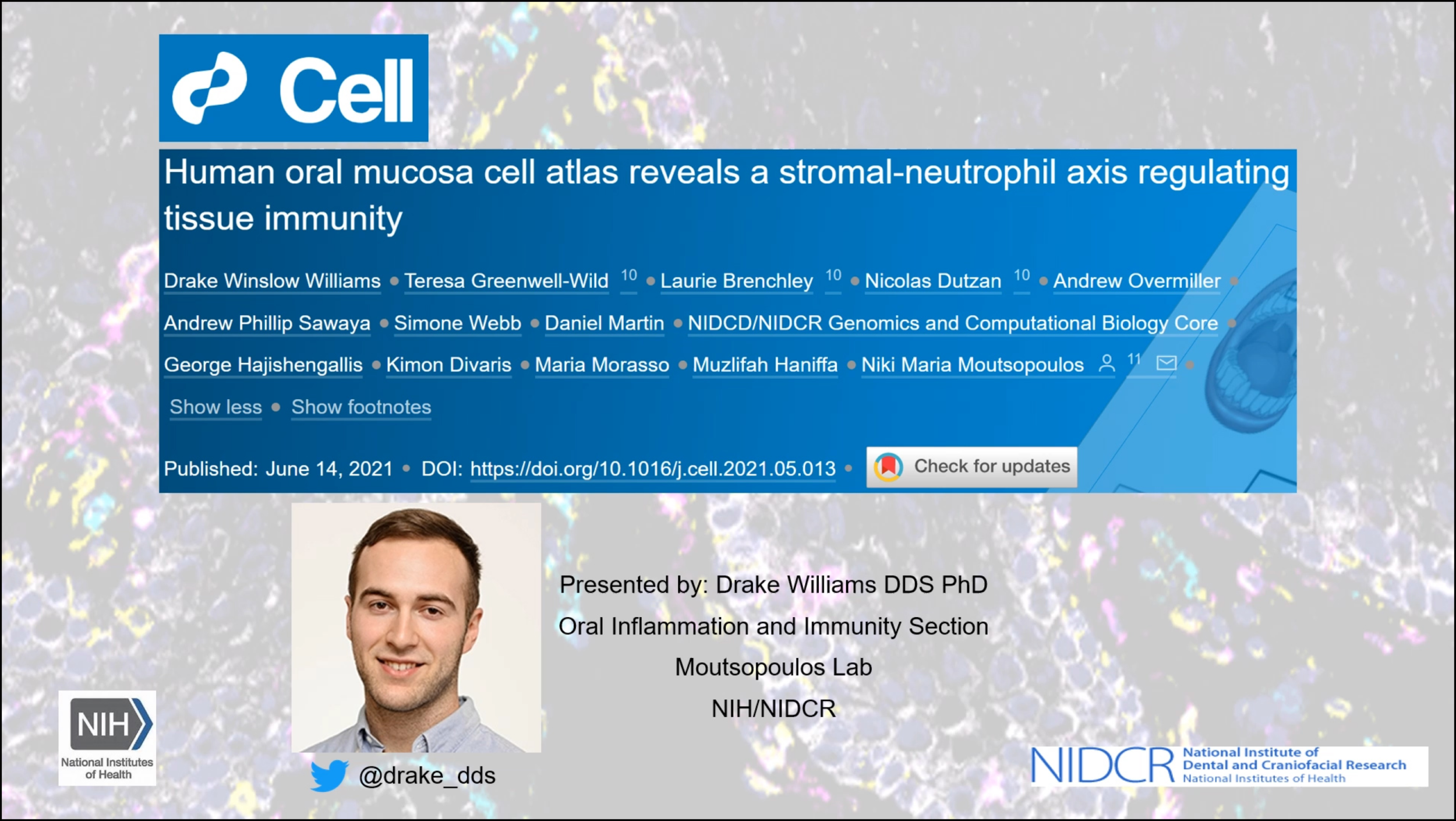
Human oral mucosa cell atlas reveals a stromal-neutrophil axis regulating tissue immunity
Drake Winslow Williams1, Teresa Greenwell-Wild1, Laurie Brenchley1, Nicolas Dutzan2, Andrew Overmiller3, Andrew Phillip Sawaya3, Simone Webb4, Daniel Martin5, NIDCD/NIDCR Genomics and Computational Biology Core5, George Hajishengallis6, Kimon Divaris7, Maria Morasso3, Muzlifah Haniffa8, Niki Maria Moutsopoulos9
- Oral Immunity and Inflammation Section, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD 20892, USA.
- Oral Immunity and Inflammation Section, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD 20892, USA; Faculty of Dentistry, University of Chile, Santiago, Chile.
- Laboratory of Skin Biology, National Institute of Arthritis and Musculoskeletal and Skin Diseases, NIH, Bethesda, MD 20892, USA.
- Biosciences Institute, Newcastle University, Newcastle upon Tyne NE2 4HH, UK.
- Genomics and Computational Biology Core, National Institute on Deafness and Other Communication Disorders, Bethesda, MD 20892, USA.
- University of Pennsylvania, Penn Dental Medicine, Department of Basic and Translational Sciences, Philadelphia, PA 19104, USA.
- UNC Adams School of Dentistry and Gillings School of Global Public Health, University of North Carolina, Chapel Hill, NC 27599, USA.
- Biosciences Institute, Newcastle University, Newcastle upon Tyne NE2 4HH, UK; Wellcome Sanger Institute, Wellcome Genome Campus, Hinxton CB10 1SA, UK; Department of Dermatology and NIHR Newcastle Biomedical Research Centre, Newcastle Hospitals NHS Foundation Trust, Newcastle upon Tyne NE2 4LP, UK.
- Oral Immunity and Inflammation Section, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD 20892, USA. Electronic address: nmoutsop@mail.nih.gov.
Abstract
The oral mucosa remains an understudied barrier tissue. This is a site of rich exposure to antigens and commensals, and a tissue susceptible to one of the most prevalent human inflammatory diseases, periodontitis. To aid in understanding tissue-specific pathophysiology, we compile a single-cell transcriptome atlas of human oral mucosa in healthy individuals and patients with periodontitis. We uncover the complex cellular landscape of oral mucosal tissues and identify epithelial and stromal cell populations with inflammatory signatures that promote antimicrobial defenses and neutrophil recruitment. Our findings link exaggerated stromal cell responsiveness with enhanced neutrophil and leukocyte infiltration in periodontitis. Our work provides a resource characterizing the role of tissue stroma in regulating mucosal tissue homeostasis and disease pathogenesis.
Presented By Drake Williams | ORCID iD